A Circle of Life day10/12/2016 (Trigger warning: miscarriage/stillbirth) So yesterday was day number…whatever…of this last call block. I’m off call today, going to a writing conference (ECWC). But before I could leave for ECWC, there was work to be done, and yesterday pushed the emotional and physical limits of my patients and me. Doesn’t help that I have a whopper of a cold. Yeah, no one wants to acknowledge it, but doctors get sick. Especially when I see every coughing, booger-oozing toddler in a twenty-mile radius for the past two weeks. And those same sick toddlers like to sneeze directly on me, or grab at my face with those grabby, snotty, glistening, crusty little hands. So that’s the background. Not at 100% to begin with on this last day of the call week. Yesterday. Phone rings at 6:30am. It’s the ER. 20 week patient has delivered a fetus literally 2 minutes ago in the ER, and the patient is bleeding badly. My head spins. Is it my patient? If so, which one? ER doc doesn’t give a name. Just asks me to get there quickly. I go from REM sleep to fully awake in 5 seconds and provide a few orders before pulling on clothes and hurrying to the hospital. En route, I’m thinking through hemorrhage protocols and meds, and also planning for the non-clinical things that need to be done to help the patient through such a devastating event. In the ER, the patient room is swarming with very uncomfortable nurses and ER doctor. (Side note: ER personnel? They truly hate anything vaguely obstetric. It’s one of those universal truths. Makes them squiggly. Fair enough. I can relate. Multi-victim traumas…not my cup of tea.) So I walk in the room and peek at the patient. Please don’t judge, but I had the brief thought, “Thank God I don’t know her.” Because the situation is, like, 100x harder if it’s someone I know. Of course, the patient is screaming and crying and her spouse is also distraught. Bless their hearts, but the ER staff has put the fetus in a basin in the sink, because they don’t know what to do and that’s okay. No one is comfortable in this situation. No one. I first assess the bleeding. Part of the placenta is out, part is still inside the uterus. What I see looks yellowish and infected. The rest has to be removed or she’ll get septic. While we’re getting set up to go to the OR, there’s that non-clinical piece to address. So I pick up the limp, red, tiny baby out of the sink and wrap…him? yes, him…up in a towel to make it look like a receiving blanket, how a regular baby would look. Because guess what? Up until a few minutes ago, this was this couple’s hopes and dreams and future and joy. It was their baby. Still is. He looks like he’s sleeping, face relaxed, translucent and veiny hands folded one over the other on his chest. I can’t absorb the sadness in this room or I won’t be able to do the technical part of the job. A thin wall goes up. It has to. My chest hurts. I ask her if she wants to hold her baby. I put my arm around her shoulders but cannot do more. I can taste the sadness. She has to hold baby with one arm while lab tech pulls stat labs from the other arm. I’d like to give this couple more time to mourn. I’d like to give them privacy. But she’s bleeding and possibly infected. There is still one living patient to take care of. After a few minutes, we roll down to the OR. The last thing I see is the baby’s father sitting on a rolling stool in the empty ER room. There are smears of hastily-wiped blood still on the floor. His face is creased and lost. In his arms is this big towel bundle with a tiny red face peeking out. I wish I had more time and more reserves to help him, too. We finish the procedure and I go talk with the father. I have to ask the question no one wants to ask. Can we send baby for an autopsy to try and find out what happened? No parent should ever have to hear the word autopsy and baby in the same sentence. Ever. Home to shower and very late arrival at the office. Before going to the OR, I had called ahead to my office and cancelled two hours of office patients. I flip on the computer at my desk and immediately see two angry patient emails. These are people who wanted to be seen today but had to be moved because of the emergency. My generous colleagues had offered to see these people, but the patients were mad at me because I wasn’t there for them during the time they had planned. There’s no good response. I ask the scheduler to offer my apologies and put them in over lunch or at the end of the day, if they would like. Second patient of the day, God love him, is a simple, nice man. He is always happy. He brings me candy, as he often does, and the first thing he says when I walk in the room, is that he’s glad to see me. How I held my shit together in front of this very kind person, I have no idea. Somehow I managed to address his health issues and lab results and tried to stay pleasant and happy. Because time with each patient is important. They want an engaged, friendly person helping them. Their priority is their own health, and they want me to share that priority, at least for the 20 minutes we spend together. Totally understandable. Next patient is an Ob patient. She’s contracting at 39 weeks and getting uncomfortable. God help me, but I calculated the probability of her delivering tomorrow morning, right as I needed to turn over call. I started thinking about things like being late for my flight. She’s only 3 cm and baby is still high in the pelvis. I send her home to walk because that is the right thing to do medically-speaking. Lunch. I’m numb, sitting in the break room, voices of nurses and techs swirling around me. Someone asks me a question. I say something like “Great, thanks.” And a few minutes later, I leave to go check on the morning miscarriage patient over the remainder of the lunch break. The chaplain has just left the patient's room. Everything about that room feels thick and dark, like emotional shades have been pulled. However rough I might feel in that space, it must only be a fraction of how my patient and her spouse are feeling. Mid-afternoon. I’m keeping one eye on the Labor and Delivery patient list, expecting and frankly dreading to see the 39 week patient’s name pop up. I feel like a jerk because that’s what I’m thinking. I also cannot breathe through my nose and have chills. Thanks, snotty toddlers from a week ago, whoever you are, you little petri dishes of pestilence and plague. A few patients into the afternoon and now I’m telling someone that their pancreatic lesion may not have a cure. We have to have a talk about 3 Wishes and Living Will and quality of life vs quantity of life. It’s too much information for him to process. He is quiet and stunned. And I see this adult patient in front of me, but my mind’s eye sees a tiny red face surrounded by a white towel. My chest hurts. Next patient. An Ob patient at 20 weeks. Irrational anxiety ratchets up. I cannot get to the handheld fetal Doppler fast enough to check for heart tones. At the end of the office schedule, I return to see the miscarriage patient. Her face is drawn, but resigned. She is feeling physically better, but you can feel the emptiness around her. I ask the questions about sadness and grief, and counseling and support services. She’s still blank. Too much information. We’ll have to revisit these questions next week back in the office. Driving home, I don’t go directly there but drive around town, up and down streets. It’s like, if I keep driving, maybe I can get some feeling back in my numb face, my numb mind. An hour later, the Ob department calls. 39 weeker is admitted, in labor. On my patient list, the miscarriage patient from the morning is still in the hospital and her name comes up right under this 39 weeker’s name. That fact makes me feel twisted up inside. Then I look at the clock and start calculating how late this delivery will be. I go to the hospital at 9pm and evaluate her. It’s going to be a late night. Two hours later, she’s pushing. And an hour after that, after an adrenaline dumping shoulder dystocia that needs to be resolved, she delivers a beautiful, healthy baby boy. He waits a full minute before he moves. That minute lasts a year in my soul. Then he screams for all he’s worth. It’s 11:55 pm. I place this slimy, pinkish, wiggly screaming child on the patient’s chest and finish my work. Mother and father cry different tears than I saw from the couple this morning. Family cheers. After hugs and handshakes, I finish notes and go home. It’s like I’ve become two people inside. I pray for no more phone calls until 7am when the call ends. There’s not a lot of reserves left inside me to help people. The feeling when I checked in at the airport this morning to do 5 days of absolutely nothing medical? Not bliss, exactly. But relief. The tightness in my chest loosens up a bit. Normally I’m super happy. Normally I have funny things to say. Maybe with the change in scenery, I can think and write about something else for a few days. Like silly characters, or impossible descriptions in novels, or chap stick, or shopping. Leave a Reply. |
Jillian DavidAuthor, daydreamer, and practitioner of trying very hard to duct tape folks together and help when I can. Archives
May 2024
March 2024
October 2023
July 2023
June 2023
April 2023
December 2022
September 2022
August 2022
June 2022
May 2022
February 2022
January 2021
November 2020
August 2020
July 2020
May 2020
January 2020
November 2019
September 2019
August 2019
July 2019
March 2019
November 2018
October 2018
September 2018
July 2018
June 2018
May 2018
April 2018
March 2018
January 2018
December 2017
November 2017
October 2017
September 2017
August 2017
July 2017
May 2017
April 2017
March 2017
February 2017
January 2017
December 2016
November 2016
October 2016
September 2016
August 2016
July 2016
June 2016
May 2016
April 2016
March 2016
February 2016
January 2016
December 2015
November 2015
October 2015
September 2015
August 2015
July 2015
June 2015
May 2015
April 2015
March 2015
February 2015
January 2015
December 2014
November 2014
October 2014
September 2014
August 2014
July 2014
June 2014
Categories
All
Adventures With Hubby
Airports
Author Interviews
Cats
Fastdrafting
Funny Medicine
Hell's Valley Series
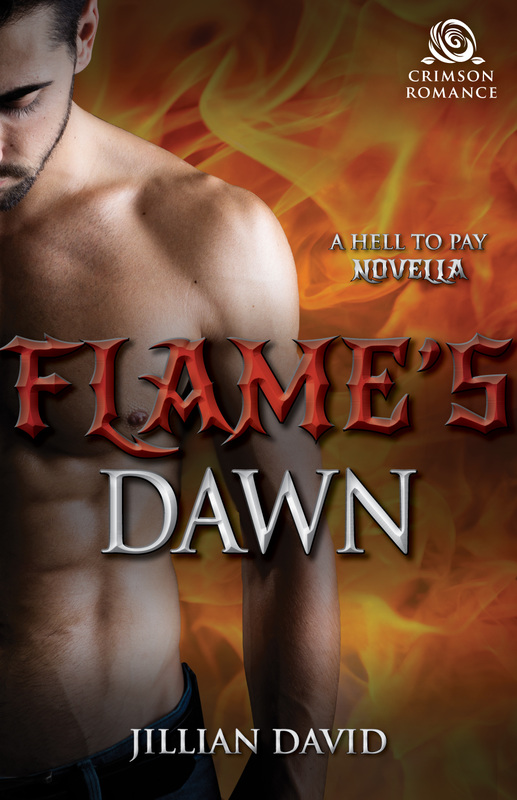
Hell To Pay Series
Medicine
Potpourri
Star Trek
Top 10 Lists
Writing
Writing Vs Medicine
Yukon Valley Hospital
|






 RSS Feed
RSS Feed